Wound Healing: A Complex Process Requiring Coordination of Multiple Cell Types
Wound healing is an intricate process involving the spatial and temporal synchronization of various resident and recruited cell types. This blog post summarizes recent advances in our understanding of the cellular and molecular mechanisms underlying normal and impaired wound healing, with implications for plastic surgery.
Overview of Wound Healing Phases
Wound healing progresses through overlapping phases of hemostasis, inflammation, proliferation, and remodeling. Effective healing requires a coordinated cellular response at each phase:
- Hemostasis: Platelets aggregate and degranulate, releasing cytokines to initiate the inflammatory response. Coagulation factors crosslink platelets into a fibrin clot that stops bleeding.
- Inflammation: Neutrophils and macrophages phagocytize debris and pathogens and release growth factors. Macrophages transition from a pro-inflammatory to a pro-healing phenotype.
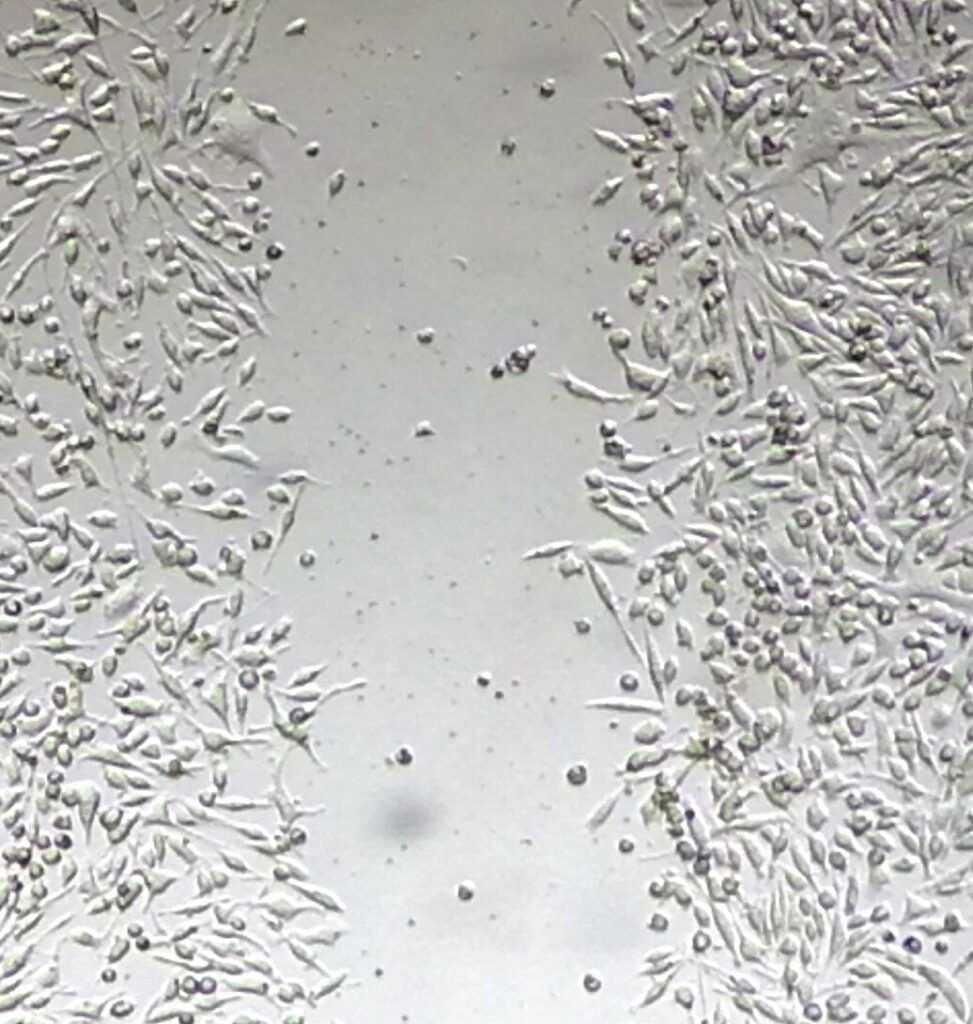
- Proliferation: Fibroblasts proliferate and differentiate into myofibroblasts, contracting the wound. Endothelial cells, pericytes and progenitor cells stimulate angiogenesis. Keratinocytes migrate and proliferate to re-epithelialize the wound.
- Remodeling: Macrophages removes dead cells and debris. Myofibroblasts undergo apoptosis. New blood vessels regress. Collagen remodeling strengthens the tissue.
Molecular Regulation of Cellular Responses
- Growth factors like PDGF, TGF-β, VEGF, and FGF orchestrate wound healing by stimulating cellular proliferation, migration, differentiation, and angiogenesis.
- ECM components such as fibronectin and hyaluronic acid provide structure and signaling cues to modulate cellular responses.
- Chemokines like MCP-1 govern immune cell recruitment to the wound site.
- Integrins facilitate cell-ECM interactions necessary for migration and mechanotransduction.
Heterogeneity of Wound Healing Cell Types
Recent advances reveal heterogeneity within wound healing cell populations:
- Endothelial cells – Tip and stalk cells perform distinct roles in angiogenesis. Endothelial cells interact with pericytes and immune cells through receptors like ανβ3, VCAM-1, and ICAM-1.
- Pericytes – Identity and origins remain unclear. May arise from mesenchymal stem cells. Support new vessels through physical interactions and ECM deposition.
- Fibroblasts – Distinct lineages based on anatomical location and developmental origin. Subsets proliferate and differentiate into contractile myofibroblasts at varied rates.
- Macrophages – Display dynamic pro-inflammatory, pro-healing, and fibrolytic phenotypes over time. Subsets uniquely interact with fibroblasts, keratinocytes and T cells.
- Dendritic Cells – Epidermal Langerhans cells and dermal DC subsets differ in T cell activation. Recruited pDCs secrete IFNα/β.
- T Cells – Diverse roles for αβ and γδ T cells. DETCs support re-epithelialization. TH2 cells implicated in fibrosis.
Impaired Wound Healing
Factors contributing to dysfunctional healing in chronic wounds and hypertrophic scars:
- Prolonged inflammation – Persistent neutrophils and M1 macrophages cause tissue damage. Delayed efferocytosis and clearance. Chronic inflammatory mediators.
- Reduced angiogenesis – Hyperglycemia alters endothelial cell function. Lower VEGF/FGF levels. Microvascular complications.
- Cellular dysfunction – Hyperglycemic memory alters progenitor cells even after glycemic control. Fibroblasts less responsive to hypoxia. Impaired macrophage stimulation of angiogenesis.
- Excessive fibrosis – Increased myofibroblast survival. Mechanotransduction via FAK/integrins enhances fibrotic signaling. Accumulation of specific fibroblast subsets.
Implications for Plastic Surgery
- Understanding heterogeneity of wound healing cells enables identification of specific targets for therapy
- Isolating pro-regenerative cells using surface markers detected by single cell analyses could improve cell-based treatments
- Determining alterated wound healing mechanisms in diseases like diabetes allows prevention of chronic wounds and scarring
- Modulating the transition between macrophages subsets may reduce fibrosis and optimize scarring
- Targeting mechanotransduction pathways could prevent or treat abnormal scarring
In summary, a thorough understanding of the coordinated cellular dynamics governing normal and pathological wound healing is important to guide effective treatments in optimizing skin repair and regeneration.
References:
Ozgok Kangal MK, Regan JP. Wound Healing. [Updated 2023 May 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK535406/
Rodrigues M, Kosaric N, Bonham CA, Gurtner GC. Wound Healing: A Cellular Perspective. Physiol Rev. 2019 Jan 1;99(1):665-706. doi: 10.1152/physrev.00067.2017. PMID: 30475656; PMCID: PMC6442927.

