The anterolateral thigh (ALT) flap has become a workhorse flap for soft tissue reconstruction in plastic and reconstructive surgery. First described in 1984 by Song et al, the ALT provides thin, pliable fasciocutaneous tissue with a long and versatile vascular pedicle. With careful dissection and flap design, the ALT flap can be customized to provide sensate coverage for defects throughout the body. This article will provide an in-depth overview of ALT flap anatomy, dissection techniques, flap variations, and clinical applications to master use of this important reconstructive tool.
Key features of the ALT flap:
- Tissue composition: skin, fat, and fascia that can be thinned or customized based on needs
- Arterial supply: descending branch of lateral femoral circumflex artery
- Vein(s): accompany artery, can be dissected to origin for pedicle length up to 8cm
- Flap dimensions: up to 25 x 8 cm, wider possible with grafting
- Innervation: lateral femoral cutaneous nerve
Anatomy and Blood Supply
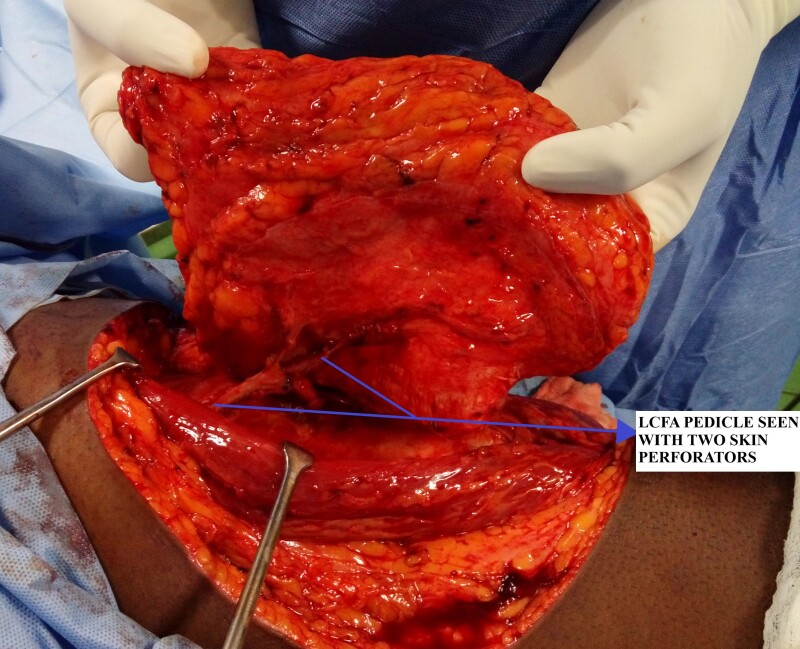
The ALT flap is supplied by perforators from the descending branch of the lateral circumflex femoral artery (LCFA). This vascular pedicle arises from the profunda femoris branch of the femoral artery. As it descends in the thigh, the LCFA gives off perforating branches that supply the overlying anterior thigh tissue. ALT flap perforators course through the septum between the rectus femoris and vastus lateralis muscles. Frequently, perforators may travel within the rectus femoris or vastus lateralis muscles.
The descending branch of the LCFA has an external diameter of 1.5-2.5mm in adults. Venous drainage parallels the artery as 2-3 veins that coalesce into a single venous pedicle near the origin. Vein diameter is slightly larger than the artery. With proximal dissection, pedicle length up to 8-10cm can be obtained.
The flap is also supplied by the lateral femoral cutaneous nerve (LFCN), which provides sensory innervation. The LFCN enters the flap near the anterosuperior border and can be dissected proximally as part of the neurovascular pedicle.
Flap Design and Dissection
The flap is designed along the axis from the anterosuperior iliac spine to the superolateral patella. Doppler ultrasound helps identify perforators through the fascia along this axis. The flap width depends on the laxity of anterior thigh tissues for closure. Flaps up to 8-10cm wide may be closed primarily, while wider flaps require skin grafting of the donor site.
The anterior surface of the flap is elevated first in the subfascial plane. Any visible perforators are preserved. The posterior flap is then raised, again preserving perforators penetrating the vastus lateralis muscle.
The septum between the rectus femoris and vastus lateralis is examined for intramuscular perforators. When present, these can provide the pedicle while sparing muscle disruption. Otherwise, the dominant perforators through vastus lateralis are dissected through the muscle to reach the descending LCFA vessels.
Pedicle Dissection and Flap Harvest
Once the dominant perforators are identified, the pedicle is fully dissected by separating the rectus femoris and vastus lateralis muscles. The artery and veins are freed proximally to the branching point of the LCFA. The LFCN is identified and can be included with the pedicle. Additional motor branches to vastus lateralis can be preserved to minimize donor site morbidity.
The flap is then completely islanded on the pedicle vessels. Flap dimensions are tailored to the requirements of the defect, with the proximal two-thirds used for larger flaps. The skin, fat, and fascia can be included for soft tissue reconstruction. For added pliability, the flap may be thinned by removing excess fat and fascia. The adipofascial layer alone can be harvested as a thin fasciocutaneous flap.
Donor Site Closure
Closure of the donor site begins by undermining surrounding tissues for mobilization. The fascia is closed with interrupted absorbable sutures followed by deep dermal sutures to relieve tension on the skin. The skin can then be closed with interrupted sutures or staples. Quilting sutures may be used to reduce potential dead space. A light pressure dressing and closed suction drain are applied.
Clinical Applications
The thin, pliable nature of the ALT flap provides excellent reconstructive options throughout the body. Some common uses include:
- Head and neck – oral cavity, tongue, pharynx, facial resurfacing
- Upper extremity – soft tissue coverage for trauma, burns, etc.
- Lower extremity – soft tissue reconstruction for trauma, chronic wounds
- Breast reconstruction – autologous tissue, stacked flaps
- Trunk – chest, abdomen, back, groin
- Perineum – vulva, vagina, penis, scrotum
- Pelvis – pressure sores, radiation damage
The ALT flap has advantages of robust and consistent anatomy, long pedicle length, good caliber vessels, and the ability to customize thickness and dimensions. However, the descending branch perforators can have variability. Meticulous technique is needed when dissecting through muscle to identify and preserve the pedicle vessels.
References:
Song YG, Chen GZ, Song YL. The free thigh flap: a new free flap concept based on the septocutaneous artery. Br J Plast Surg. 1984 Apr;37(2):149-59. doi: 10.1016/0007-1226(84)90002-x. PMID: 6713155.
Alexander L, Fahrenkopf MP. Free Tissue Transfer of the Lateral Thigh and Anterolateral Thigh. [Updated 2022 Sep 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK563253/
MICROSURGEON.ORG (no date) The Anterolateral thigh (ALT) flap. Available at: https://www.microsurgeon.org/anterolateralthigh (Accessed: 02 October 2023).

